CMS Extends Meaningful Use Hardship Extension Where Vendor Delayed with Certifying EHR Technology.
CMS Extends Meaningful Use Hardship...
Copiers result in $1.2 million settlement and CAP for Affinity Health
Copiers result in .2 million settlement and CAP...
Document Disposal Company Responsible for old Patient Records found in Park
Document Disposal Company Responsible for old...
WellPoint hit with $1.7 million for Security Weaknesses in Online Application
WellPoint hit with .7 million for Security...
ONC Sells Successes of Health IT Adoption to Congress in Annual Report
ONC Sells Successes of Health IT Adoption to...
Lessons from the Idaho State University CAP
Lessons from the Idaho State University CAP ...
ONC Releases Governance Framework for Trusted HIE
ONC Releases Governance Framework for Trusted...
EHR Vendor Loses Meaningful Use Certification
EHR Vendor Loses Meaningful Use...
Proposed Rules Extend EHR Donation Sunsets for Stark and Anti-Kickback
Proposed Rules Extend EHR Donation Sunsets for...
The ACA SCOTUS Decision in Plain English
The ACA SCOTUS Decision in Plain English ...
CMS Releases Additional Meaningful Use Guidance for EPs; Stage 3 Recommendations Underway
CMS Releases Additional Meaningful Use Guidance...
FDA Moving Forward with Regulating Mobile Health Apps
FDA Moving Forward with Regulating Mobile Health...
CMS Releases New Meaningful Use FAQ for EPs using Hospital EHRs
CMS Releases New Meaningful Use FAQ for EPs...
OCR Releases HIPAA Audit Protocol as Audits Continue
OCR Releases HIPAA Audit Protocol as Audits...
The $1.7 Million Flashdrive…Alaska Medicaid Settles HIPAA Violations
The .7 Million Flashdrive…Alaska Medicaid...
HITECH Omnibus Rule Out by End of Summer
HITECH Omnibus Rule Out by End of Summer ...
Mass. AG Levies 750k Judgment on Hospital for Data Breach
Mass. AG Levies 750k Judgment on Hospital for...
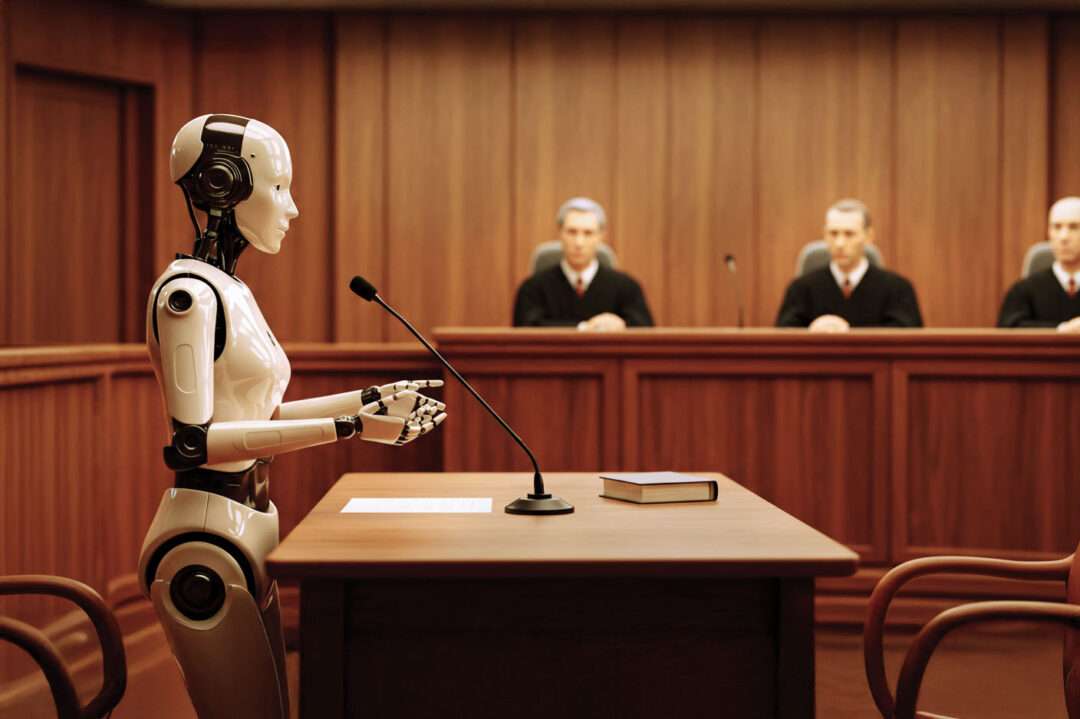
Will HIPAA Conviction Appeal Loss Open the “Zhou” Gates?
Will HIPAA Conviction Appeal Loss Open the...
Are We Ready for the Nationwide Health Information Network? ONC Releases RFI for Governance of NwHIN
Are We Ready for the Nationwide Health...
Legal and Practical Implications of Meaningful Use Attestation
Legal and Practical Implications of Meaningful...
We “Like” Organ Donor Status on Facebook
We “Like” Organ Donor Status on Facebook This...
Subscribe & Survive the onslaught of new healthcare regulations requiring updates to affected compliance programs.
Get access to exclusive subscription-only access to resources, tools, industry analysis and other valuable solutions.